ADULT & CHILD HEALTH AWARDED $3.9 MILLION IN GRANT FUNDING FOR MENTAL HEALTH AND SUBSTANCE ABUSE SERVICES EXPANSION
Grant Will Establish Adult and Child Health as a Certified Community Behavioral Health Center INDIANAPOLIS (Feb. 9, 2021) – The Substance Abuse and Mental Health Services Administration (SAMHSA) has announced Adult and Child Health (A&C) has received a two-year, $3.9 million grant to expand and enhance behavioral health services in Marion and Johnson counties. This grant, funded in part by the CARES Act, enables Adult and Child Health and nine other Indiana centers to operate as Certified Community Behavioral Health Centers (CCBHCs). With the additional funding, A&C will implement more comprehensive mental and substance use treatment by adopting CCBHC service standards – an integrated and financially sustainable model for care delivery. Created by the National Excellence in Mental Health and Addiction Treatment Expansion Act, the purpose of the CCBHC program is to increase access to mental health and substance use treatment while also treating co-occurring primary care concerns. RELATED CONTENT: Adult & Child Health Receives $321,000 Grant from Lilly Endowment to Support Youth Services under COVID-19 “We’re grateful to SAMHSA for the award and to our partners at the state for supporting the CCBHC model of care, said Allen Brown, President and CEO of Adult and Child Health. “Indiana is leading with the number of mental health centers that have CCBHC designation. We’re confident outcomes will show that the CCBHC approach is a superior model for the mental health and addictions safety net.” As a CCBHC, A&C’s services will include same-day behavioral health care, mobile crisis services, treatment with medication for opioid use disorder, primary care health screenings, community-based treatment, case management and care coordination with community partners that serve veterans, children, and those involved with the justice system. “The grant couldn’t come at a better time for A&C. Along with the COVID-19 hardships people are facing, we’re seeing record levels of depression, anxiety, and addiction,” said Dan Arens, Adult and Child Health’s Chief Operating Officer. “This funding creates access to critical services for the people who absolutely need it the most.” Target populations for CCBHC services include individuals with serious mental health or addiction, including opioid disorders; children and adolescents with serious emotional disturbance; and individuals with co-occurring physical health disorders. CCBHCs provide person- and family-centered services to any individual in need, regardless of their ability to pay or their place of residence. Adult & Child Health is a community mental health center and Federally Qualified Health Center (FQHC) Look Alike that offers primary care and behavioral health services. We strive for caring communities, where every child, adult and family have the opportunities they need to live healthy, happy, productive lives. For more information about Adult & Child Health services, please contact Adam Wire, marketing and communications specialist, at 317-882-5122.
ADULT & CHILD HEALTH RECEIVES $321,000 GRANT FROM LILLY ENDOWMENT TO SUPPORT YOUTH SERVICES UNDER COVID-19

INDIANAPOLIS (Nov. 18, 2020) – Adult & Child Health (A&C), an Indianapolis-based nonprofit that supports the mental, physical, and social health of Central Indiana youth, has received a $321,000 grant through the Lilly Endowment Inc.’s Youth Program Resilience Fund. A&C Health’s specialized staff work 1-on-1 to improve the behavioral health and well-being of nearly 7,000 at-risk youth and families every year and provide face-to-face services in youths’ homes, classrooms, and community settings. Since the onset of COVID-19 in March, A&C staff have rapidly adjusted their programming for youth by implementing socially distanced and telehealth methods of service delivery. That flexibility, while allowing the agency to safely support the behavioral needs of youth throughout the pandemic, has come at significant financial cost. A&C will use the Lilly Endowment grant funding to offset pandemic-related expenses, assuring that youth services continue and are delivered in ways that are medically safe for youth and staff. RELATED CONTENT: Adult & Child Health Receives Kendrick Foundation Grant to Provide Support for Morgan County Students in Response to COVID-19. “We’re very grateful to the Lilly Endowment for helping us support and protect our staff so that they may, in turn, support community youth during the pandemic,” said Allen Brown, CEO of Adult & Child Health. “We’re seeing a dramatic increase in the demand for services. The grant fills a critical financial need as we adapt to serve high-needs youth in a COVID-19 environment.” Funding from the Lilly Endowment Inc.’s Youth Program Resilience Fund will allow A&C Health the flexibility to provide a safe and healthy balance between supporting youth with ongoing face-to-face and telehealth-based care while also meeting the personal health and safety needs of staff. Assistance from the grant will be used to support youth program staffing, purchase resources for telehealth service delivery, and provide Personal Protective Equipment (PPE) for youth-serving staff providing in-person services. RELATED CONTENT: Adult & Child Health Awarded $3.2 Million Grant to Expand Mental Health Services for the Homeless Adult & Child Health strives for caring communities, where every child, adult and family have the opportunities they need to live healthy, happy, productive lives. For more information about Adult & Child Health services, please contact Adam Wire, marketing and communications specialist, at 317-882-5122. Lilly Endowment Inc. is an Indianapolis-based, private philanthropic foundation created in 1937 by J.K. Lilly and his sons, Eli and J.K. Jr., through gifts of stock in their pharmaceutical business, Eli Lilly and Company. The Endowment supports the causes of community development, education, and religion, and it maintains a special commitment to Indianapolis and Indiana.
Overcoming Trauma: The Power Behind Skills Development and Therapy
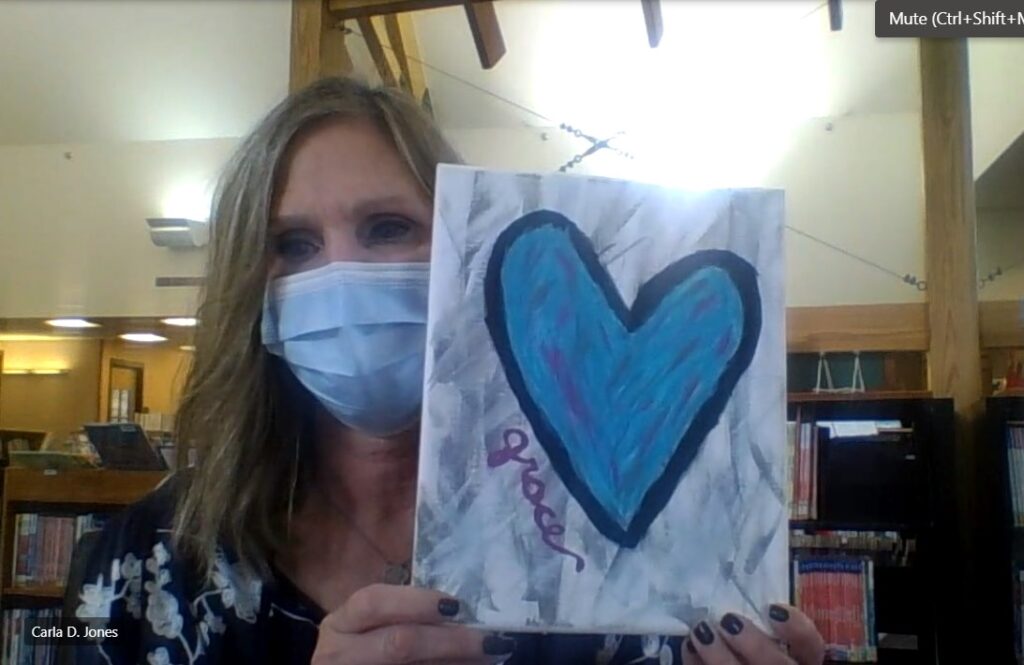
When I first met Angela Wood, it wasn’t surprising how well-spoken, engaging and self-assured she is. Anyone who meets her would tell you the same thing. They certainly wouldn’t notice any skills development needs. That exterior appearance belies everything she’s endured in recent years. It also inspired her artwork that currently hangs in the lobby of Adult & Child Health’s primary care clinic in downtown Indianapolis. “I can decorate, but I’m not good at art,” Wood said, even though her artwork suggested otherwise. “I prayed about it, and it was really special. The Lord put a picture in my head of what I could display. I went through some terrible trauma … I’m just so grateful to breathe when I wake up in the morning.” RELATED CONTENT: A&C Launches Telehealth to Serve Wheeler Mission Guests The painting and its meaning Every component of Wood’s painting, “Grace,” is intentional. The heart’s black border represents her trauma. The lighter shade of blue inside the heart “was the Lord showing me that my heart was full of color, light and hope again. So I wanted to make the inside brighter and cheerier,” she said. Trauma doesn’t seem visible when you meet Angela. But as she tells her story, though, you begin to understand there’s plenty of it. Angela suffered a traumatic brain injury (TBI) five years ago, the victim of a domestic violence incident, which she said almost killed her. She was hit on the back of her head with a metal base. The injury didn’t seem life-threatening at first, but as time passed, she began to notice cognitive issues. “I didn’t tell anyone (at first) because I was scared; I didn’t go to the hospital,” Angela said. “Things were getting harder for me. I would freeze up; had trouble showering. My son and sister were trying hard to help me. One morning, I woke up to get ready for work and could not move. I called my boss and went unconscious during the call. I was exhausted; couldn’t think straight. My son and boss came to my house and called the ambulance.” RELATED CONTENT: I Took Mental Health First Aid Training. Here’s Why You Should, Too. How skills development improved her life After Angela was released from the hospital about five years ago, her brain function hadn’t improved enough to make her self-sufficient, so she went to Wheeler Mission. During her time there, she hooked up with A&C and Carla Jones for skills development assistance. She’s still seeing Carla, five years later, about once a week. “They saved my life,” Wood said of Jones and Kelsey Schrank. Jones serves as Wood’s Skills Development Specialist, and Schrank works as her Therapist. “I could not have recovered without that support. Carla has helped me grocery-shop again and cook. When we first started, I had a lot of trauma reappear. I had a lot of panic attacks and nightmares, but then I started moving forward again. She helped me with the communication piece. I saw trauma affecting my communication. We would go places together, and then we’d evaluate how I did and what I said; not to let my triggers and anxiety affect me when I’m out in society. I feel like I’m doing a lot better now.” Jones enjoys working with Angela and helping her improve. “I’m very thankful to even have this opportunity to be her skills development specialist to be able to assist her to build resiliency skills and improve her overall quality of life,” Jones said. “I’m just glad to be here with her through it.” Schrank admires Wood for acknowledging her issues, and the bravery she’s shown addressing them. “TBI and trauma are very similar,” Schrank said. “From the outside looking in, someone might not know. To that person, it’s a very real experience and there’s a lot of shame involved in that. She’s doing a great job of describing something that’s a hard thing to survive.” How therapy is helping alongside skills development While Jones helped Angela with the practical, everyday-life side, Schrank assisted with the attack’s emotional effects. “Kelsey helped me so much with confidence and self-care,” Angela said. “I was so used to taking care of others, I didn’t realize how I wasn’t taking care of myself. The (domestic) relationship as it became toxic was taking me. It wasn’t letting me be who I am. I’m healthy. I have peace and joy again. I can be who I was created to be without stress.” Wood said Shavon Donald has also been instrumental in her ongoing recovery, because she’s felt thankful to have a supportive psychiatrist who believes in her and her recovery process. Do want to help us help others live healthier lives? Here’s how to donate. What’s next for Angela Angela recently reunited with her family. She has two sons and a daughter, all adults, and she hopes to spend time with her two young grandchildren soon. Angela’s transformation has awed Schrank. “When we first started working together, I heard Angela often express that backward-looking view. When will I get back to the old me? Recently, I’ve heard such an evolution. She’s excited about the future. You can see how recovery brought about new opportunities for her.” Angela wants to teach a yoga class or own a yoga studio someday, or possibly reach out to others on their own recovery journey. “That’s kind of my new passion.” But not artwork? “My first response was, ‘Oh no, my artwork isn’t going to be amazing, but it’s not what it looks like, it’s what it meant to me,” Wood said. “I hope my artwork touches someone else that there’s a light at the end of the tunnel.” Are you having a mental health crisis, or do you know someone who is? Call our Open Access Crisis Line at 1-877-882-5122.
A Q&A with Adult & Child Health COO Dan Arens about Telehealth Transition

When the COVID-19 pandemic hit, it affected virtually every aspect of our lives. The virus forced health care agencies to adapt and adjust like no other entities. Clients were suddenly encouraged into quarantine, reducing their ability and willingness to access primary care and behavioral health care visits. Employees felt equally insecure in providing a service that has always been, until recently, face to face. Adult & Child Health, like nearly everyone else, needed to evolve quickly or risk leaving thousands of under-resourced men, women, and children without access to care. In late February and early March, when COVID-19 began spreading to the U.S. and Indiana, A&C’s leadership was paying close attention. On March 13, when schools began to close their doors and transition to e-learning, A&C effectively transitioned 95% of its medical, psychiatric and counseling service visits from in-person to telehealth delivery models with very minimal loss of client engagement. RELATED CONTENT: A&C Launches Telehealth to Serve Wheeler Mission Guests How we transitioned to telehealth Adult & Child Health Chief Operating Officer Dan Arens oversaw much of the transition process and relied heavily on the expertise of A&C’s leadership teams and direct care staff who really drove the hard work. “It was so amazing to see the lengths to which our staff were willing to go to make sure our clients were still being taken care of,” he said. “Our 70-year face-to-face business model was upended and re-designed in a matter of weeks. That’s a remarkable testament to what can be accomplished by a mission driven team.” He shared his thoughts on the transition process, how it’s working today and what it means for the agency and health care in the future. Q: Which changes we’ve made to our health care services and access in the wake of COVID-19 do you think will be temporary, and which ones will remain permanently? A: “Since the on the onset of COVID in mid-March, A&C has effectively transitioned our services from a face to face model to a televideo model and kept the large majority of our patient base engaged in services. From skills development work in the schools, to homeless services, family therapy, registration, and medical services, for the most part, access to our full continuum of care has remained intact via televideo. “We’ve found televideo to be a very effective tool under the pandemic circumstances. The decision to continue these services under a telehealth model really falls to our payors. Under COVID-19, the rules around telehealth billing have been relaxed; if those rules continue to allow telehealth, A&C Health would be happy to continue to offer services under the telehealth model. I suspect, access to some services under telehealth will remain permanently (i.e. therapy, acute medical/psych visits, etc), while others will return to face-to-face only.” Q: Is telehealth actually preferable to our traditional in-person patient visit model? If so, why? A:“Our clients have really adjusted well to the telehealth model. I believe people appreciate the option; especially those with mobility, transportation, work schedule, or other barriers to care. That said, every client is different in their comfort level with telehealth. In an industry based so heavily upon building relationships, discussing emotionally difficult topics, and working across support networks, telehealth does present its own set of challenges. Our staff have been really creative in these areas during this emergency, but I believe a mix of face-to-face and telehealth options is the best solution.” RELATED CONTENT: Our Foster Care Services Are Still Here for You During COVID-19. Here’s How We’re Doing It. Q: We serve a specific population compared to traditional health care facilities/agencies. Will telehealth be beneficial to our client demographic long-term, and if so, why? A: “Many of our clients do experience multiple barriers to care; perhaps moreso than traditional health care. Telehealth certainly does expand our clients’ options for access to care. Beyond the common barriers like transportation, telehealth does afford us a different approach to treating people who experience mental health challenges that make it difficult for them to attend services in person. “I believe telehealth has also allowed our agency to reduce the number of clients who present at ER’s for non-emergent services. Whether for primary care or behavioral health services, telehealth has allowed us to be more nimble in working urgent care patients into same-day visits.” Q: What changes do we still need to make as an agency (or as an industry) to make telehealth a viable long-term health care access option? A: “Long term, I believe COVID-19 has forced us all into telehealth models and we’ve collectively demonstrated the remarkable benefit of telehealth. Insurance payors, providers, and patients adapted really quickly. As with any new process, we have some work flow adaptations we’re working to implement, which will improve client care, follow up, registration efficiencies. The beneficial components of face-to-face health care (like connectivity, body language, empathy, compassion, etc.) don’t translate as effectively via tele-video. Those aspects of the visit are very important to good care, so we, as an industry, will need to find creative ways to keep these traits present in a tele-visit model.” Q: How have our clients responded to telehealth? Not just in terms of individual feedback, but participation in the process (i.e. have no-shows increased, decreased or remained flat)? A: “We’ve not had a chance to do a patient satisfaction survey and compare pre-COVID versus during-COVID statistics, but I can say our no-show rate has gone down, clients have voiced appreciation that A&C is still providing care. Many other mental health, substance use, and safety net providers closed their doors for weeks at a time due to COVID, leaving people without care. I’m very proud of our staff’s dedication to serving our clients. When a 600(ish)-person agency transitions from a full face-to-face service model to a 95% telehealth service model in about 10 days, you know you have staff who care about those they serve.” This chart (at left) clearly demonstrates the successful transition of visits in our clinics from



